
Step 1
Donor patient
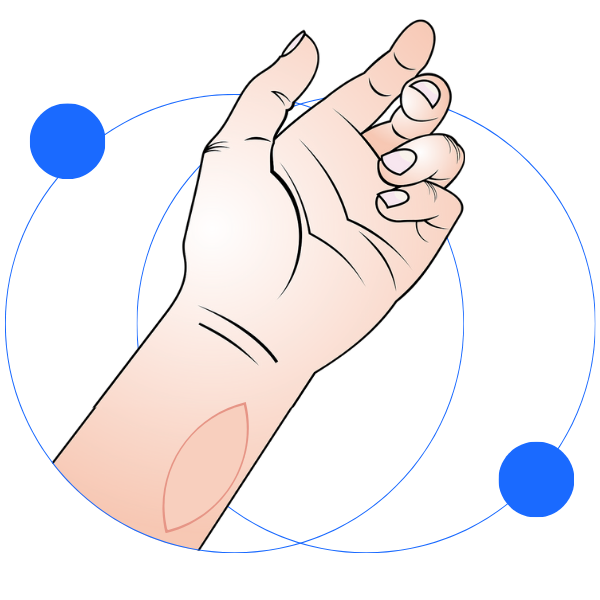
A small patch of skin (with its blood supply) is taken from the forearm of the same donor at the same time of the organ transplant.
Step 2
During organ transplantation
The skin is transplanted onto the patient’s forearm — this is called the Sentinel Skin Flap. The flap heals leaving a small visible patch on the forearm.

Step 3
Monitoring
Transplanted skin displays signs of rejection early, any rejection is often seen visually as a rash. Patients and healthcare workers can both check the flap regularly, and in some cases patients may be asked to share photos during follow-up.

Step 4
Action
Once rejection is spotted, doctors can adjust treatment — often preventing major complications. A small biopsy of the skin flap can confirm rejection.
The Procedure
Four steps of the Skin Flap procedure
Understanding the process
One of the major issues with organ transplantation is when the immune system attacks the new organ. This process is called acute rejection, and it can cause patients to become unwell and lead to organ failure.
We are investigating a new technique for transplant patients that allows a more rapid detection of organ rejection following transplant. The technique is called a Sentinel Skin Flap (SSF).
This involves transplanting a small patch of skin (eye-shaped and the size of two fingers together) from the same organ donor patient onto the forearm of the recipient patient at the same time they receive the organ transplant.
If immune system rejection of the new organ develops, a rash appears on the skin of the SSF. The skin offers the advantage of being easily visualised, allowing both patients and doctors to appreciate changes in appearance 24/7. This rash may indicate early rejection in transplanted organ and prompt treatment may prevent organ damage.
The goal is simple: detect rejection earlier, treat it faster, protect the transplanted organ, and give patients greater peace of mind.

Why it matters
1. Early signal
Visible rashes appear on the skin before symptoms of organ damage occur.
2. Simpler biopsies
If confirmation is needed, a small skin biopsy from the flap is minimally painful, carries less risk than a solid-organ biopsy, and requires fewer hospital resources.
3. Patient involvement
Patients can take an active role by monitoring their flap.
4. Better outcomes
Treating rejection early helps protect the transplanted organ and may help the transplanted organ stay healthier for longer.
